Introduction:
Bile Matters: Delving into Causes, Navigating Complications, and Simplifying Diagnosis
In the intricate landscape of human health, understanding the nuances of bile-related issues is crucial. This article, “Bile Matters: Delving into Causes, Navigating Complications, and Simplifying Diagnosis,” aims to unravel the complexities surrounding these conditions, offering valuable insights into the causes, complications, and simplified diagnostic approaches.
What are the complications of excess Bile Matters?
Excess bile production or issues with bile flow can lead to various complications. Bile plays a crucial role in the digestion and absorption of fats, and any imbalance in its production or secretion can result in health problems. Here are some potential complications of excess bile:
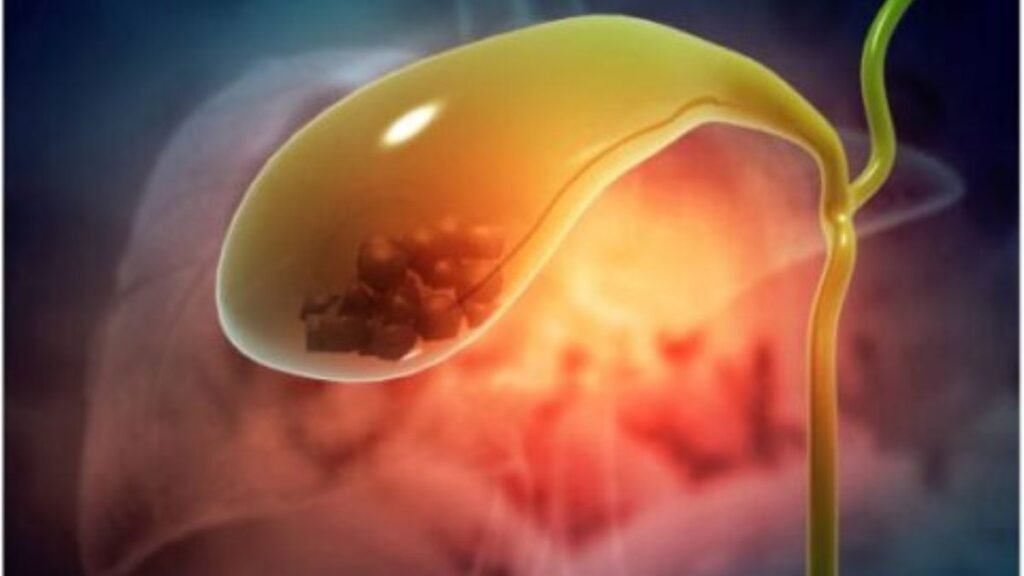
- Gallstones: Excess bile can contribute to the formation of gallstones. Gallstones are solid particles that can develop in the gallbladder due to an imbalance in the substances that make up bile, such as cholesterol and bilirubin.
- Biliary Colic: Increased bile production or an obstruction in the bile ducts can cause biliary colic. This condition is characterized by sudden and intense pain in the upper abdomen, often after consuming a fatty meal.
- Cholecystitis: Excessive bile can lead to inflammation of the gallbladder, a condition known as cholecystitis. This inflammation can be caused by the presence of gallstones or an infection.
- Pancreatitis: Bile duct obstruction can lead to pancreatitis, inflammation of the pancreas. The pancreas produces digestive enzymes, and if these enzymes are not properly transported to the small intestine due to bile duct obstruction, they can start to damage the pancreas itself.
- Malabsorption of Fat: Bile is essential for the emulsification and absorption of fats in the small intestine. If there is an excess of bile, it can interfere with the normal absorption of fats, leading to malabsorption issues and deficiencies in fat-soluble vitamins (A, D, E, and K).
- Diarrhea: Increased bile in the intestines can cause irritation and lead to diarrhea. Bile acids can act as laxatives and contribute to the loosening of stools.
- Jaundice: If there is an obstruction in the bile ducts or liver dysfunction, excess bilirubin (a component of bile) can accumulate in the bloodstream, causing jaundice. Jaundice is characterized by yellowing of the skin and eyes.
- Digestive Issues: Excess bile can contribute to various digestive issues, including indigestion, bloating, and discomfort after eating.
It’s important to note that the specific complications may vary depending on the underlying cause of the excess bile, such as gallbladder dysfunction, liver disease, or other gastrointestinal conditions. Individuals experiencing symptoms related to excess bile should seek medical attention for proper diagnosis and management.
How is bile reflux diagnosed?
Bile reflux is diagnosed through a combination of medical history, physical examination, and various diagnostic tests. Here are some common methods used by healthcare professionals to diagnose bile reflux:
- Medical History and Symptoms Evaluation:
- The doctor will begin by taking a detailed medical history, including a discussion of your symptoms. Bile reflux symptoms may include heartburn, regurgitation, abdominal pain, and discomfort.
- Physical Examination:
- A physical examination may be conducted to assess overall health and identify any signs of complications related to bile reflux.
- Endoscopy:
- Upper gastrointestinal endoscopy is a common procedure used to visualize the esophagus, stomach, and duodenum. During an endoscopy, a flexible tube with a light and camera (endoscope) is passed through the mouth and into the digestive tract. This allows the doctor to examine the lining of the esophagus and stomach and identify any signs of inflammation, irritation, or damage caused by bile reflux.
- Esophageal pH Monitoring:
- pH monitoring involves placing a small tube through the nose into the esophagus to measure the acidity levels over a 24-hour period. This test helps determine whether stomach acid or bile is refluxing into the esophagus and assesses the frequency and duration of reflux episodes.
- Esophageal Manometry:
- This test measures the strength and coordination of the muscles in the esophagus. It helps assess the function of the lower esophageal sphincter (LES), the muscle that separates the esophagus from the stomach and helps prevent reflux.
- Imaging Studies:
- Imaging tests, such as a barium swallow or upper gastrointestinal series, may be performed to visualize the upper digestive tract. These tests involve swallowing a contrast material that can be seen on X-rays, allowing the doctor to identify any abnormalities.
- Gastric Emptying Study:
- In some cases, a gastric emptying study may be conducted to assess the rate at which the stomach empties. Delayed gastric emptying can contribute to bile reflux.
- Bile Acid Tests:
- Specialized tests may be performed to measure bile acid levels in the stomach or esophagus. These tests can help confirm the presence of bile reflux.
It’s important to note that the diagnostic process may vary based on the individual’s symptoms and the healthcare provider’s preferences. If you are experiencing symptoms suggestive of bile reflux, it is advisable to consult a healthcare professional for a thorough evaluation and appropriate diagnostic testing.
What is the best treatment for bile reflux?
The treatment for bile reflux depends on the underlying cause and the severity of symptoms. Here are some common approaches used to manage bile reflux:
- Lifestyle and Dietary Modifications:
- Avoiding trigger foods and making changes to dietary habits can be helpful. This may include reducing the intake of fatty and fried foods, chocolate, caffeine, and alcohol. Eating smaller, more frequent meals and avoiding lying down after meals can also be beneficial.
- Medications:
- Proton pump inhibitors (PPIs) and H2 blockers are medications that can help reduce the production of stomach acid, which may alleviate symptoms of bile reflux. However, they may not be as effective in treating bile reflux as they are in treating acid reflux.
- Bile Acid Sequestrants:
- Medications known as bile acid sequestrants may be prescribed to bind bile acids in the stomach and prevent them from entering the esophagus.
- Promotility Medications:
- Medications that enhance the movement of the digestive tract (prokinetic agents) may be prescribed to improve the emptying of the stomach and reduce the chances of bile reflux.
- Antacids:
- Antacids can provide temporary relief by neutralizing stomach acid. However, they may be less effective against bile reflux compared to acid reflux.
- Surgery:
- In severe cases or when other treatments are ineffective, surgical intervention may be considered. Surgical procedures may include fundoplication, which involves wrapping the top of the stomach around the lower esophagus to reinforce the lower esophageal sphincter (LES), or bile diversion surgery to redirect bile flow away from the stomach and esophagus.
- Endoscopic Therapy:
- Endoscopic procedures, such as the placement of stents or the injection of bulking agents, may be used to treat bile reflux in some cases.
- Treatment of Underlying Conditions:
- Addressing underlying conditions that contribute to bile reflux, such as gallbladder dysfunction or liver disease, may be an essential part of the treatment plan.
It’s crucial to consult with a healthcare professional to determine the most appropriate treatment based on individual circumstances. The choice of treatment will depend on factors such as the specific symptoms, the underlying cause of bile reflux, and the overall health of the individual. Additionally, a comprehensive evaluation may be necessary to rule out other gastrointestinal conditions and ensure an accurate diagnosis.
Conclusion:
Empowering Health Decisions “Bile Matters” concludes by emphasizing the importance of awareness and proactive healthcare decisions. By unveiling the causes, navigating complications, and simplifying diagnosis, this article serves as a valuable resource for individuals seeking to understand and manage bile-related diseases effectively.
Remember, staying informed is the first step towards a healthier future. Explore the comprehensive insights provided in “Bile Matters,” and empower yourself to make informed decisions for your well-being.